A bipartisan group of lawmakers introduced legislation that would force the breakup of pharmacy benefit managers (PBMs), the drug industry middlemen that have come under increasing scrutiny by lawmakers and regulators.
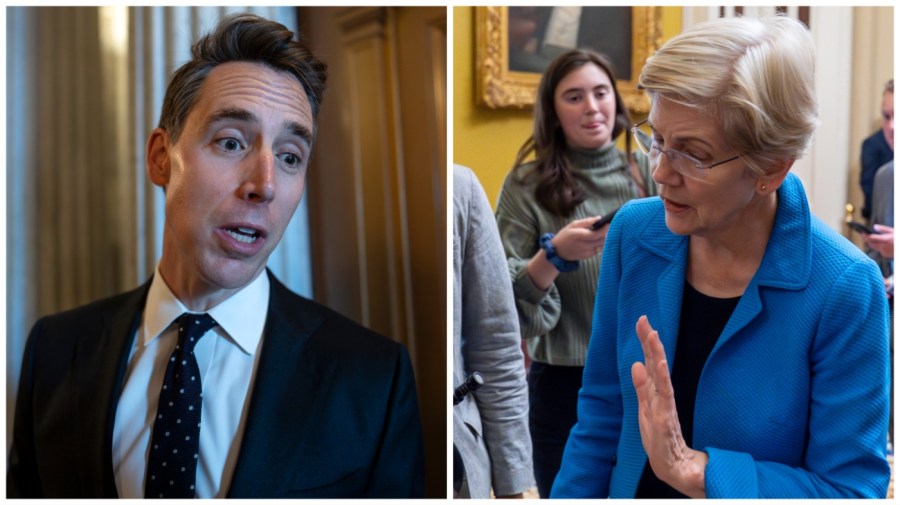
A Senate bill led by Sens. Elizabeth Warren (D-Mass.) and Josh Hawley (R-Mo.) would prohibit a parent company of an insurer or PBM from also owning pharmacies, forcing companies to divest their pharmacy businesses within three years.
It’s a practice the lawmakers called “a gross conflict of interest that enables these companies to enrich themselves at the expense of patients and independent pharmacies.”
A companion bill in the House is led by Reps. Diana Harshbarger (R-Tenn.) and Jake Auchincloss (D-Mass.)
PBMs are on the hot seat, as lawmakers and regulators dig into what they say are the perverse incentives within the industry that drive up drug prices.
“PBMs have manipulated the market to enrich themselves — hiking up drug costs, cheating employers, and driving small pharmacies out of business,” Warren said in a statement.
PBMs negotiate the terms and conditions for access to prescription drugs for hundreds of millions of Americans. They are responsible for negotiating prices with drug companies, paying pharmacies and creating formularies that determine which drugs patients can access and how much they cost.
As the industry has grown more consolidated, critics say PBMs have exerted greater control over patients’ access to medicine. PBMs are vertically integrated, serving as health plans and pharmacists.
The three biggest PBMs—CVS Health’s Caremark, Cigna’s Express Scripts and UnitedHealthGroup’s OptumRx—are owned by insurance companies, which in turn also own specialty, mail order or retail pharmacies.
PBMs and brand drug manufacturers negotiate rebates — volume-based discounts for plans and pharmacies — which the PBM then passes on to employers. The industry argues they help keep costs contained and insurance premiums low.
But a Federal Trade Commission investigation found PBMs also impose restrictions that limit access to less expensive drugs and inflate the cost of cancer drugs. A report by House Republicans had similar findings, and also explored how PBMs charge patients more to use their local pharmacy as a way to steer patients to the PBM-affiliated ones.
“The insurance monopolies are ruining American health care. Patients and independent pharmacies are paying the price. This legislation will stop the insurance companies and PBMs from gobbling up even more of American health care and charging American families more and more for less,” Hawley said in a statement.
It’s likely too late in the year for the bill to advance, but the bipartisan effort shows lawmakers are trying to lay the groundwork for reform next year. President-elect Trump has also indicated he backs efforts to crack down on PBM business practices.
There are efforts to include a provision in the year-end spending bill that would change how PBMs are paid in order to eliminate an incentive to drive patients to the highest-cost drugs.
Last summer, Harshbarger and Auchincloss teamed up for a bill targeting PBMs attempts to steer patients to their preferred pharmacies.
But Wednesday’s legislation, if passed, would represent the most significant attempt yet to regulate the industry.